Thursday, April 30, 2020
Wednesday, April 29, 2020
ASDA’s efforts in response to COVID-19
“Has your school begun mandating self-quarantines?”
“Have you had any COVID-19 cases in your state yet?”
Instead of the usual, “How was your flight?” or “Are you ready to graduate?” these were the questions that I was greeted with by friends from all over the country at ASDA’s Annual Session in St. Louis last month. At the time, I had the very naive thinking that this was all an overreaction. Of course, lobby day 2020 would take place on the Hill and the 2020-21 national ASDA councils would seamlessly transition into their new roles at the Spring Council leadership meeting in Chicago. I would also be walking across the graduation stage in May. However, I soon began scratching each of these exciting and important items off of my calendar as COVID-19 moved across the country.
What is comforting to know in this time of disappointment and uncertainty, is that ASDA has been by the side of dental students every step of the way. Two of the main issues we are facing as dental students are concerns over finances (particularly student loans), as well as the postponement of licensure examinations and experiences needed for graduation.
In regards to the first point, ASDA sent letters to Speaker Nancy Pelosi, House Minority Leader Kevin McCarthy, Senate Majority Leader Mitch McConnell and Senate Minority Leader Charles Schumer asking for legislation that accomplished two things. The first was deferment of interest on all federal student loans for dental students and dental residents. The second was deferment of all monthly payments on federal student loans for dentists without penalty. With the Coronavirus Aid, Relief, and Economic Security (CARES) Act, signed into law at the end of March, federal student loan borrowers will not be required to make a payment on their loans and no interest will accumulate through Sept. 30.
For my fellow dental students in their final year, I know this is an especially challenging time in regards to the postponement of licensure examinations and experiences needed for graduation. There is no definitive great news yet; however, while ASDA is fighting every day for you, it is even more exciting to see grassroots advocates all over the nation stand up and help lead the charge to graduation. Licensure reform is way overdue, and this current crisis is a good time to drive the conversation forward.
At ASDA, we are delivering a unified message that dental schools and educators should be looking for alternative ways to ensure their students graduate on time. We also continue advocating for alternative pathways to initial dental licensure that do not include a live patient. We are pleased to report ASDA’s collaboration with the American Association of Dental Boards, ADEA and regional testing agencies have led to an accelerated release of many agencies’ manikin-based clinical examination.
- On March 26, Western Regional Examining Board (WREB) announced an internal work group to fast track a non-patient-based exam to be implemented this year due to exceptional circumstances.
- On April 1, the Central Regional Dental Testing Services (CRDTS) announced the release of their all-manikin exam. This exam is an option for the periodontal and restorative procedures traditionally administered on a patient.
- On April 6, the American Board of Dental Examiners (ADEX) announced its release of the CompeDont DTX. It is a non-patient-based restorative examination that uses the CompeDont
 DTX, a new manikin tooth technology developed by the CDCA and Acadental, Inc.
DTX, a new manikin tooth technology developed by the CDCA and Acadental, Inc. - On April 13, the Southern Regional Testing Agency (SRTA) announced the release of their manikin-based restorative skills module using cutting-edge dental products that are highly effective in simulating a live patient’s dental procedures.
Furthermore, on April 2 the ADA Joint Commission on National Dental Examinations approved the release of the Dental Licensure Objective Structured Clinical Examination (DLOSCE), which will be available for use in June 2020. ASDA is working with district trustees and local ASDA leaders on a state-by-state licensure strategy, urging state dental boards to accept these alternative pathways to initial dental licensure for 2020 graduates.
ASDA is committed to being the voice of dental students all over the nation now more than ever, despite the setbacks and cancellation or postponement of all in-person meetings. It breaks my heart to not be standing on Capitol Hill with you all this spring, continuing to push the field of dentistry to new and better heights. However, I know you are all being incredibly fierce advocates every day during this difficult time. What an incredible time to unite and push the conversation forward on issues such as licensure reform and student debt, which seem to be getting the attention they deserve. Keep advocating, and I will see you all on Capitol Hill in 2021.
~Kate McPherson, North Carolina ’20
Tuesday, April 28, 2020
Monday, April 27, 2020
ADEA PASS application: What you need to know
Applying to residency is a daunting experience, like applying to dental school all over again. You’re stuck wondering if you’ll get accepted, what you’ll do if you aren’t accepted and what the requirements are for each program that you’re planning on applying to include. In trying to keep track of all of these different applications and requirements, it’s super easy to get overwhelmed or bogged down.
The American Dental Education Association Postdoctoral Application Support Service (known as ADEA PASS) was created to mitigate some of these stresses. Listed below are some facts about the PASS application, as well as some tips and tricks on how to use it to help you have a stress-free experience while applying to residency programs.
- What is the PASS application for? The PASS application is basically used as a centralized system, comparable to the Common Application or AADSAS. The PASS application allows you to submit one application for the multiple programs that you will most likely be applying to for residency. The PASS itself includes over 700 advanced dental education programs, encompassing all specialties.
- When does it open, and when should it be completed? The PASS application opens each year around mid-May. Applications for the 2020-21 cycle will open May 14, 2020.There is ample time to fill it out, as it doesn’t close until Feb. 8, 2021. That being said, it is always beneficial to submit your applications early. You never can be too careful when submitting an application so important to your future. With any computer-based application, there are always processing times, and you don’t want these to delay your application.
Keep in mind, you also need to be checking on the dates for submission of applications to each individual residency program. Just because the PASS application closes in February, does not mean that you have that long to submit your application for an individual program you’re interested in.
- What do you need to have ready? The most important first step in applying to residency through the ADEA PASS application is to make sure you figure out if the program(s) that you want to apply to participate in the application. Although there are over 700 participating programs, this does not guarantee the program you’re applying to is one of them. As far as physical materials you will need, you should have your transcripts, test scores (when applicable) and letters of recommendation ready to go.
Outside of that, requirements vary program to program, and it’s important to look into each one to see what else they require. A great way to do this is by visiting the ADEA PASS Search Engine, which allows you to look up programs and see the program contact, deadline and other information (i.e. requirements, supplemental fees, length of program, etc.)
- What does it cost? The first program that you apply to through ADEA PASS will cost you $195 and then each successive program is $89. Keep in mind that individual programs might have fees outside of this through the PASS app (similar to AADSAS). If your program requires a background check, this will also have a fee of around $100.
Applying to residency can be a stressful experience, but hopefully the ADEA PASS application can mitigate some of that for you so that you can focus on patients instead of what materials you need to submit and where to submit them. For more specific questions, definitely reach out to someone you know who has used the PASS application or visit ADEA’s website.
~ Lauren Young, Detroit Mercy ’22, Chapter Outreach Chair
Friday, April 24, 2020
Thursday, April 23, 2020
Wednesday, April 22, 2020
How embracing my two cultures impacted me as a dental student
I am an immigrant, and I am a dental student. I was born in one country and raised in another. I’m also the first of anyone in my family to pursue a career in dentistry.
There are a lot of things new to me and my family right now, but we are adjusting well like we always have.
We moved to the United States when I was 2 years old. From then, I’ve been constantly adapting to something new and different. While now I am learning to assimilate into the dental world, growing up, I had to learn to assimilate into American culture.
In elementary, middle and high school, I fully embraced my Korean culture at home and only at home. I watched Korean TV shows with my parents, listened to K-pop and obsessed over Korean celebrities with my sisters. At school, I had to be American. I couldn’t talk about my favorite Korean TV show of the season or my favorite foods because my friends would not have been able to relate. In elementary school, I hated when my mom would pack me Korean food because of the comments, stares and scrunched noses. Yet as I made more friends and as times in America changed to better accept different cultures bit by bit, I was able to find an identity in both of my cultures.
My family, friends and personal experiences have molded me and helped me define my identity. I tried so hard for many years to be my own definition of “all-American” and pushed my Korean culture aside. Now, I identify as a Korean American. Depending on the setting, sometimes the Korean side of me comes out stronger than the American side or vice versa, but I never forget about either one. I take pride in having roots in two places, and there is beauty in being able to take part in two cultures, two sets of traditions and knowing two worlds.
Finding my identity was not that quick and easy, though. During this time of acclimating to American life together, my parents and I grew apart in a way because I was adjusting far faster than they were. They already had deeper roots in Korean culture, while I was just starting to find mine here, in America. Growing up, my friends had sleepovers from which I was always picked up early. Dating was OK only if I was at an age to be able to get married — my current apartment in Augusta is still just a temporary dormitory in my parents’ eyes.
When I was younger and more naïve, I used to think that these differences in ideas and opinions were huge roadblocks. I would get angry and frustrated with my parents because I thought they did not want to listen; now I know these were just a few examples of cultural differences that we had (and will continue to have) that we can use to build an understanding together.
As first generation in multiple aspects, I had plenty of practice venturing into the unknown alone and finding a mentor along the way. My parents and I experienced American public schooling for the first time, hand in hand. Since kindergarten, I sat down with my mother every Friday in elementary school and explained my “Friday Folders” to her in Korean. I was the translator at all of the parent/teacher meetings, and in middle and high school, continued to translate for her.
Both my parents went to college and continued their education beyond bachelors’ degrees, but that was in South Korea. Applying to American colleges was a brand new concept to us, so I sought help from school counselors and, at times, my equally confused peers.
The journey to and through dental school is not very different. I find help from resources outside of my family, but because of all the practice venturing into the unknown, I have learned to quickly adjust to changes and simply enjoy the bumpy ride of life in dental school. Today, I do not hesitate to step out of my comfort zone and embrace the thrill of finding familiarity in the unknown. The biggest difference now is that, today, I am more comfortable in my skin than ever before.
In dental school, I have deeply connected with so many classmates of different backgrounds and cultures. I have laughed and cried with them as we shared our stories. In the clinic, we cross paths with so many people from around the world and even between states and cities, and I have been able to exchange so many wonderful stories based on our different cultures. Through this, I have learned that there will be times of tension when we as students do not understand a staff member, professor or patient. In any relationship, differences in culture can be seen as difficulties. I tell myself that these are simply inconveniences disguised as barriers. With a little more understanding and patience, we can connect with patients, professors and peers with more compassion and empathy.
~YeaRim Kim, Georgia ’22, Chapter Historian
Tuesday, April 21, 2020
Monday, April 20, 2020
What you should know about endodontic microsurgery
Microsurgeries in endodontic treatment are surgical procedures performed under magnification following failure of a non-surgical root canal, also known simply as a root canal. Root canal treatment can fail for many reasons. In order to decide whether surgery is the proper treatment approach, it is important to establish the etiology of the disease.
Bacteria from the oral cavity enters the root canal system following a carious or traumatic insult to the tooth. This bacteria is then able to produce inflammation and subsequent gradual necrosis of pulpal tissue. As bacteria continues to degrade pulpal tissue, it is possible for bacteria to exit the root canal system through the apex of the tooth and cause destruction of supporting bone. The success of a nonsurgical root canal is achieved by the elimination of the effects of disease-causing bacteria within the canal system. Upon exit of bacteria through the apex of the tooth, it becomes substantially more difficult to eliminate the effects of these bacteria with traditional root canal therapy. In these cases, endodontic microsurgery presents a viable option to addressing bacterial activity on the outside of the tooth.
Nonsurgical root canal therapy is recommended in a variety of situations where the pulpal tissue has been irreversibly affected. Such damage frequently results in dental pain or non-painful sequelae within the surrounding bone. Sequence of treatment for teeth that have not been previously endodontically treated typically includes non-surgical root canal therapy followed by close monitoring and evaluation for the dissolution of associated symptoms and pathology. For teeth that have been previously endodontically treated, nonsurgical retreatment of the tooth should first be attempted in an effort to improve upon the cleaning and shaping initiated with the first root canal procedure.
Following the retreat, another period of monitoring is allowed to assess whether elimination of bacteria within the canal system allows healing. If the pathology or symptoms are not resolved, it is at this time that surgical intervention may become an option to eliminate the disease process.
Surgical options available beyond nonsurgical root canal therapy include apicoectomies and intentional replantation, often provided by endodontic specialists. Apicoectomies are performed through a carefully prepared osteotomy through buccal bone with the goal of visualizing the apex of the tooth to be treated. With adequate visibility, the end of the root is ideally resected by a measurement of 3 mm. Following resection, the root end is then prepared with ultrasonic instruments and retrofilled with a biocompatible putty material.

Intentional replant cases are similar in purpose but are essentially an apicoectomy performed extraorally. Ideal cases for intentional replantation are teeth with unresolved symptomatic periapical pathology associated with teeth distal to the first molar position. Additionally, teeth that present as ideal cases are those with conical root anatomy that can be atraumatically extracted. This procedure is time sensitive and should take place inside of 15 minutes of the tooth being out of the mouth.
In this time, the root is resected by a minimum of 3 mm, stained with methylene blue and evaluated for cracks, and retroprepped and filled. After replacement in the mouth, firm pressure is required to support acceptance of the tooth back into the periodontium.


Endodontic therapy provides an opportunity for patients to retain their natural teeth following carious or traumatic insults. When counseling patients about available treatment, it is important to present all options so that they can be properly educated to make the decision best for them.
~Francesca Daigle, Texas A&M ‘21
 Diode laser surgery can successfully treat white lesions on the lips, promoting quick healing and complete lip restoration without causing bleeding or requiring stitches, according to a recent case report published in the Cureus Journal of Medical Science.
Diode laser surgery can successfully treat white lesions on the lips, promoting quick healing and complete lip restoration without causing bleeding or requiring stitches, according to a recent case report published in the Cureus Journal of Medical Science. As we continue to make our way in uncertain times, there are things dental practices can do to ensure they continue to thrive in what could be a new normal, writes Dr. Mikaeya Kalantari.
As we continue to make our way in uncertain times, there are things dental practices can do to ensure they continue to thrive in what could be a new normal, writes Dr. Mikaeya Kalantari. Dental consultant Sally McKenzie has put together some ideas and suggestions to help dentists and team members reopen their practices in the most successful way possible following the disruption caused by the COVID-19 pandemic.
Dental consultant Sally McKenzie has put together some ideas and suggestions to help dentists and team members reopen their practices in the most successful way possible following the disruption caused by the COVID-19 pandemic.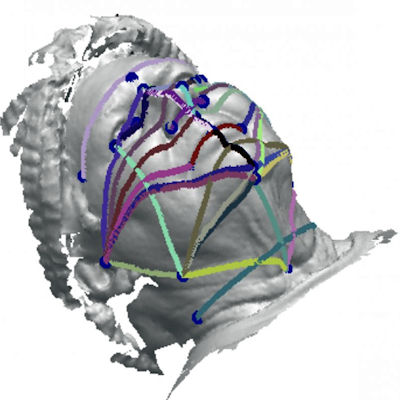
 HIPAA violations are a serious matter, leaving your dental practice feeling vulnerable. A HIPAA breach can result in thousands of dollars in fines and is potentially punishable with jail time. Robert Patrick offers advice on how to avoid eight common scenarios that can cause HIPAA violations.
HIPAA violations are a serious matter, leaving your dental practice feeling vulnerable. A HIPAA breach can result in thousands of dollars in fines and is potentially punishable with jail time. Robert Patrick offers advice on how to avoid eight common scenarios that can cause HIPAA violations. Dr. David Rice, clinical editor for DrBicuspid.com, explains why a patient's desire to spend as little time as possible in a dental practice after the COVID-19 outbreak will help push forward the technologies of CAD/CAM and 3D printing.
Dr. David Rice, clinical editor for DrBicuspid.com, explains why a patient's desire to spend as little time as possible in a dental practice after the COVID-19 outbreak will help push forward the technologies of CAD/CAM and 3D printing. As dental practices prepare to reopen across the country, Josey Sewell has some advice: Turn this hiatus from your practice into a time to play catch-up or tackle your wish list so your business is in the best possible position when it's time to reopen.
As dental practices prepare to reopen across the country, Josey Sewell has some advice: Turn this hiatus from your practice into a time to play catch-up or tackle your wish list so your business is in the best possible position when it's time to reopen. From the comfort of your own home, join DrBicuspid.com and some of the leading speakers in the dental industry on May 14-15 for the free Spring Virtual CE Conference & Trade Show. Continuing education (CE) credit will be offered.
From the comfort of your own home, join DrBicuspid.com and some of the leading speakers in the dental industry on May 14-15 for the free Spring Virtual CE Conference & Trade Show. Continuing education (CE) credit will be offered. How should dental practices be communicating with their patients and each other right now? We sat down with consultant Judy Kay Mausolf to get her thoughts on best practices and why answering the phone right now is so important.
How should dental practices be communicating with their patients and each other right now? We sat down with consultant Judy Kay Mausolf to get her thoughts on best practices and why answering the phone right now is so important.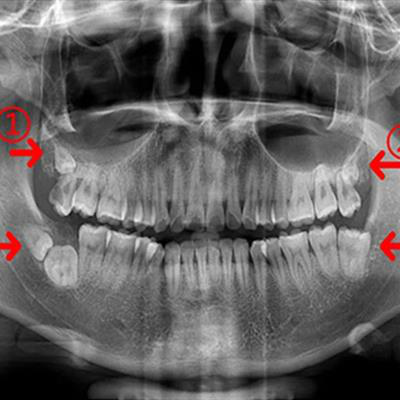 Cone-beam computed tomography (CBCT) revealed that a man had the rare dental conditions of kissing molars, bilateral distomolars, and macrodontia. An intraoral exam failed to detect the conditions, according to a case report published April 16 in BMC Oral Health.
Cone-beam computed tomography (CBCT) revealed that a man had the rare dental conditions of kissing molars, bilateral distomolars, and macrodontia. An intraoral exam failed to detect the conditions, according to a case report published April 16 in BMC Oral Health. Dental insurance expert Teresa Duncan joins DrBicuspid.com Editor-in-Chief Kevin Henry on a podcast to discuss what she is hearing about reimbursement for dental practices when it comes to personal protective equipment (PPE) in the coming days as dentists and team members start to get back to work.
Dental insurance expert Teresa Duncan joins DrBicuspid.com Editor-in-Chief Kevin Henry on a podcast to discuss what she is hearing about reimbursement for dental practices when it comes to personal protective equipment (PPE) in the coming days as dentists and team members start to get back to work. To succeed in the new dental economy, you need more than clinical skills. You also need to know how to manage a team and run your business efficiently. To get your business to the next level, search for tested, trusted methodologies you can use, says Dr. Roger P. Levin.
To succeed in the new dental economy, you need more than clinical skills. You also need to know how to manage a team and run your business efficiently. To get your business to the next level, search for tested, trusted methodologies you can use, says Dr. Roger P. Levin. With nearly 160 million Americans less than three months away from running out of money due to the burgeoning effect of the COVID-19 pandemic, 84% of people believe the U.S. government should step up and send another wave of stimulus checks, according to a new survey.
With nearly 160 million Americans less than three months away from running out of money due to the burgeoning effect of the COVID-19 pandemic, 84% of people believe the U.S. government should step up and send another wave of stimulus checks, according to a new survey. The Great Recession of 2008-2009 is not an exact analogy to the COVID-19 crisis. However, there are lessons that can be learned from the last economic downturn, especially as it appears that this one will be even deeper. Dr. Roger P. Levin gives his thoughts on the history and lessons every dentist should know.
The Great Recession of 2008-2009 is not an exact analogy to the COVID-19 crisis. However, there are lessons that can be learned from the last economic downturn, especially as it appears that this one will be even deeper. Dr. Roger P. Levin gives his thoughts on the history and lessons every dentist should know. Sugar cravings may be driven by more than just taste buds, according to a study published on April 15 in Nature. Researchers discovered sugar activated the brains of mice -- even when it was deposited straight into their guts.
Sugar cravings may be driven by more than just taste buds, according to a study published on April 15 in Nature. Researchers discovered sugar activated the brains of mice -- even when it was deposited straight into their guts. About three in four patients do not feel safe visiting their dentists for nonurgent dental treatments during the COVID-19 pandemic, according to new data released by the dental service organization North American Dental Group.
About three in four patients do not feel safe visiting their dentists for nonurgent dental treatments during the COVID-19 pandemic, according to new data released by the dental service organization North American Dental Group. Those dentists who forge ahead with technology, teledentistry, and no-insurance business models that benefit practices and patients likely will have the least rocky return from the COVID-19 disruption, says Chelsea Acosta Patel.
Those dentists who forge ahead with technology, teledentistry, and no-insurance business models that benefit practices and patients likely will have the least rocky return from the COVID-19 disruption, says Chelsea Acosta Patel. Showing how working together from afar can happen in today’s COVID-19 environment, Dr. Alvin Danenberg discusses a recent case where a patient found him over the internet and they worked together to solve the source of the patient's pain and inflammation.
Showing how working together from afar can happen in today’s COVID-19 environment, Dr. Alvin Danenberg discusses a recent case where a patient found him over the internet and they worked together to solve the source of the patient's pain and inflammation. Dr. Sheri Doniger believes many of her colleagues are feeling stressed about not doing enough during the COVID-19 pandemic. It's OK to set limits and not burn yourself out in getting ready for your practice to kick back into high gear, she says.
Dr. Sheri Doniger believes many of her colleagues are feeling stressed about not doing enough during the COVID-19 pandemic. It's OK to set limits and not burn yourself out in getting ready for your practice to kick back into high gear, she says. A whopping 46% of dentists believe they will not be able to sustain their practices if they are forced to keep postponing all nonemergency treatments through the end of August due to the COVID-19 pandemic, according to new data from the ADA Health Policy Institute.
A whopping 46% of dentists believe they will not be able to sustain their practices if they are forced to keep postponing all nonemergency treatments through the end of August due to the COVID-19 pandemic, according to new data from the ADA Health Policy Institute. How has the dental business been changed by COVID-19? Some dental assistants are wondering about going back to work, and when and if it will really be safe to do so. In this podcast, Dr. David Rice and Kevin Henry discuss some of the mental pictures they are hearing being drawn by assistants and offer their best advice.
How has the dental business been changed by COVID-19? Some dental assistants are wondering about going back to work, and when and if it will really be safe to do so. In this podcast, Dr. David Rice and Kevin Henry discuss some of the mental pictures they are hearing being drawn by assistants and offer their best advice. Clustered papular growths on a woman's lips led to a diagnosis of a rare, genetic condition that's associated with an increased risk of breast cancer and other cancer types, according to a case report published in the April 9 issue of the New England Journal of Medicine.
Clustered papular growths on a woman's lips led to a diagnosis of a rare, genetic condition that's associated with an increased risk of breast cancer and other cancer types, according to a case report published in the April 9 issue of the New England Journal of Medicine. Before you open the doors again, evaluate what worked and what didn't work before the COVID-19 pandemic. Now is the time to update the practice, train the team, and set new goals or evaluate current ones, writes Dr. James Anderson.
Before you open the doors again, evaluate what worked and what didn't work before the COVID-19 pandemic. Now is the time to update the practice, train the team, and set new goals or evaluate current ones, writes Dr. James Anderson.